1. The UCSF Health Problem
The profound impact of social and behavioral determinants of health (SBDH) on patient outcomes is well-established, with some studies citing that as much as 80% of health outcomes are driven by SBDH rather than medical care itself[1]. In response, CMS has launched a 3-step roadmap, where step 1 is to increase awareness of SBDH factors (by rewarding/penalizing patient screening rates or SBDH-1), step 2 is to address SBDH factors (by rewarding/penalizing screening positivity rates or SBDH-2), and step 3 is to improve clinical outcomes that are heavily impacted by SBDH factors (by rewarding clinical outcomes)[2]. The City and County of San Francisco have similarly prioritized addressing SBDH—particularly opioid use—due to their substantial local impact[3].
Although UCSF Health has made significant workflow changes to meet the goals of the first screening step, the latter two steps–reducing SBDH positivity rates and improving health outcomes in the presence of SBDH factors–are substantially more difficult, as they require a deep understanding of a patient’s social and behavioral needs and how it interplays with their medical needs. While the health system has always targeted these latter steps, gaps remain with current approaches. Current workflows require structured screening for at risk SBDH, however, the Department of Care Management and Patient Transitions estimates that this screening workflow may miss up to 85% of patient's with at risk SBDH. Therefore, the current workflow depends on (i) social work teams abstracting SBDH-relevant information across fragmented/unstructured charts from multiple encounters and often multiple years (akin to “finding a needle in a haystack”), searching for relevant resources that a patient is eligible for, and connecting patients to these social resources; and (ii) medical teams consulting with the social work teams to understand the social context, perhaps even conducting their own chart review, and adjusting medical care accordingly. Our vision is to drastically scale the delivery of whole-person care (i.e. addressing both social and medical needs in an integrated fashion) by building an AI-powered copilot that reduces clerical burden and facilitates targeted referrals and treatment plans concordant with patients' social and behavioral needs.
2. How Might AI Help
The Whole Person Care Navigator builds upon UCSF Health’s existing commitment to addressing SBDH and complements the recent effort to address high capacity by identifying and prioritizing patients with social needs. Current SBDH workflows at UCSF are triggered by structured data elements summarized in electronic health record (EHR) tools or obtained through manual chart review. However, most SBDH information is embedded and scattered across unstructured data elements in highly nuanced notes from the current medical encounter and historical record. In addition, SBDH information is often uncovered during unstructured discussions, and SBDH info may not be fully documented due to time constraints. With the recent advancements in large language models, we can develop an AI tool to extract SBDH information so that social workers and healthcare providers can maximize their time providing direct patient care and trigger downstream workflows. The proposed tool will (i) generate concise, patient-specific summaries highlighting social risks, previous interventions, and care gaps from both current and historical encounters, thereby reducing cognitive load and saving time previously spent on manual chart reviews; (ii) extract structured data elements for use by downstream workflows, e.g. flagging high-risk patients experiencing significant social and behavioral adversity or finding patient contacts hidden in the notes; (iii) offer personalized recommendations for relevant hospital and community resources tailored to each patient’s current and historical social circumstances and prior referral experiences; (iv) provide clinicians with actionable guidance to adjust medical treatment plans according to identified social and behavioral needs, e.g. “Given the patient’s transportation barrier, a travel voucher may help the patient attend their follow-up appointments” or “Given the patient’s financial instability, consider a 90-day supply of medications provided on discharge”[5] and (v) provide a structured data flag to the newly launched Early Screening for Discharge Planning (ESDP) and Prioritization Tool to enhance the Social Work structured data tool with the added power of AI. Given the versatility of LLMs, this tool will be easily customizable by end-users and across clinical settings.
Our team, in close collaboration with the ZSFG social worker team, has already prototyped a tool with features (i) and (ii) using PHI-compliant GPT-4o with in-context learning and internal verification via self-judging. We will work with UCSF to integrate existing databases of local and regional social resources for feature (iii) and develop with UCSF experts in social-risk informed care safe and actionable suggestions for adjusting treatment in light of patients’ social needs for feature (iv).
3. How would an end-user find and use it?
The Whole Person Care Navigator decision support tool will be embedded within a custom APeX navigator as an interactive webpage. Social workers and hospital medicine teams will receive a daily updated summary of each patient’s SBDH, including referral recommendations and decision support for social risk-informed care. This summary will appear directly beneath the patient one-liner in the Epic Sidebar, enabling situational awareness during pre-rounding and facilitating integration into medical decision-making and multidisciplinary rounds. Additionally, a direct link to the custom navigator will be accessible within the "Social Drivers" section, located below the FindHelp link in APeX. Finally, high risk flags for SBDH will be surfaced to providers via the Early Screening for Discharge Planning and Prioritization Tool.
4. Embed a picture of what the AI tool might look like
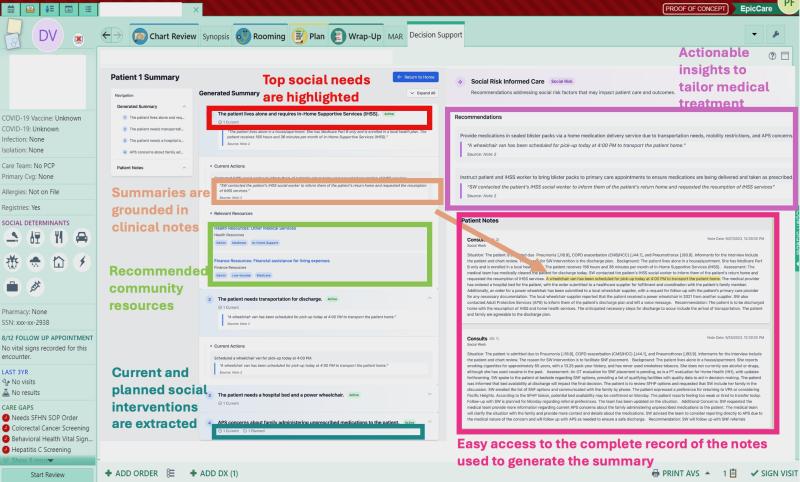
Figure 1. Anatomy of the proposed decision support tool seen embedded within a custom navigator within APeX. An interactive demonstration of the Whole Person Care Navigator tool can be found at: https://zsfg-prospect.github.io/social-wayfinder/
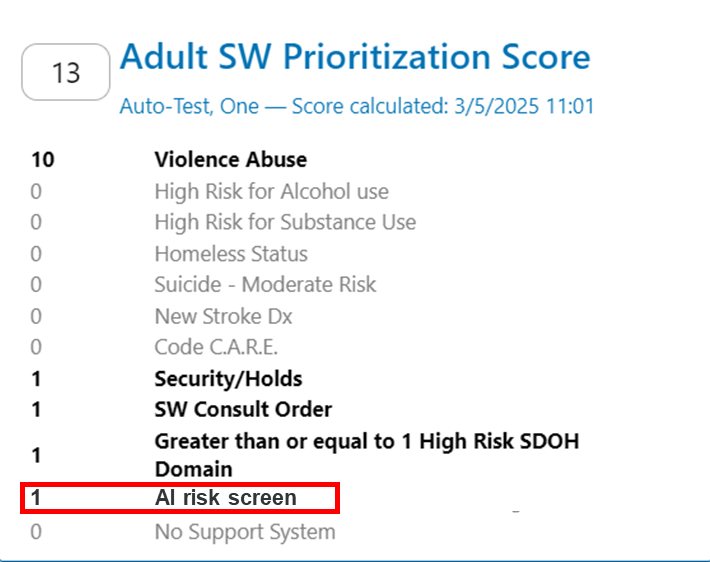
Figure 2. Example of a high risk flag generated by the Whole Person Care Navigator surfaced in the Early Screening for Discharge Planning and Prioritization Tool
5. What Are the Risks of AI Errors?
Potential risks from the Whole Person Care Navigator tool with our mitigation strategies are as follows: (i) Hallucinations and inaccuracies: To mitigate this risk, all AI-generated summaries are accompanied with direct quotations from the clinical note that can be easily verified by the user. (ii) Unhelpful social-risk informed care suggestions: To mitigate this risk, the tool will be assessed on retrospective patient cases, where its recommended adjustments will be scored by social-risk informed care experts and healthcare providers as being unhelpful vs helpful; (iii) Inequitable performance: In addition to standard validation metrics[6] for AI-generated summaries, we will test the tool within protected subgroups to ensure equitable performance. We will adjust the AI algorithm if performance differences are found. (iv) Performance drift: Our group has been designing robust monitoring systems for LLM-based tools in collaboration with IMPACC to detect performance drift. We will apply our monitoring systems to this tool as well. We will then create avenues for end users to continuously provide feedback and create a standardized training program to onboard new users.
6. How Will We Measure Success?
To validate the Whole Person Care Navigator tool, we will first conduct a pilot study focused on iterative improvement via rapid PDSA cycles with a small group of inpatient hospital medicine social workers and resident-led hospital medicine teams and then a cluster randomized trial with social workers, medicine residents and hospitalists across UCSF Health sites. The primary endpoints will be (i) time spent on chart review by social workers, as assessed through audit logs, (ii) whether the treatment plan was concordant with the patient’s social needs, as assessed through a standardized rubric using clinical notes and referrals, and (iii) the CMS screening positivity rate measure (SBDH-2). All Endpoint data are available within APeX. Secondary endpoints include the tool’s utilization rate and user satisfaction. Reasons for discontinuation would include limited adoption, negative user feedback, or persistent inaccuracies in the tool’s recommendations.
7. Describe your qualifications and commitment
This project is co-led by Dr. Lucas Zier, MD, MS, an Associate Professor in the Division of Cardiology and DoC-IT, and AI researcher with clinical appointments at ZSFG and UCSF Health, and Dr. Jean Feng, PhD, Assistant Professor of Epidemiology and Biostatistics. They co-direct the PROSPECT Lab, which aims to improve health outcomes in underserved populations through AI-based tools and whose work has received national recognition including the CAPH/SNI Quality Leaders Award and the Joint Commission Tyson Award for Excellence in Health Equity. Drs. Zier and Feng have developed and deployed five large scale EHR-integrated decision support tools and led retrospective, prospective, and randomized trials at both ZSFG and UCSF Health assessing these tools. This project is supported and will be advised by Sarah Imershein, Senior Strategy Consultant for the Care Management and Patient Transitions Department, Natalia Kelley, Nurse Informatacist and UCSF social work leads Meher Singh and Timothy Chamberlain.
7. Summary of Open Improvement Edits
We have made the following revisions to the proposal based on feedback and comments:
- We have clarififed that the Whole Person Care Navigator will draw upon internal UCSF SBDH resource databases to provide patient specific recommendations.
- We have addedd Figure 2 to demonstrate how high risk flags for SBDH will be surfaced to providers via the Early Screening for Discharge Planning and Prioritization Tool.
Additional clarifications about the prosposal in response to comments and questions:
- We appreciate the feedback about adding qualitative interviews to assess faciliators and barriers to use of the tool. Our build process includes interative human centered design with subject matter experts in the development phase and we have experience performing rapid qualitative interviews in the post deployment/optimaization phase. Therefore we could include this both for providers using the tool and for patients.
- We appreciate the question about flexibility and customization of this tool. we agree that this could be expanded into the Emergency Department to assist with the management of opiate use disorder with small changes to the underlying prompts. This flexibility and customization we believe is a stregnth of this approach.
- We regards to questions about end user testing and importance of this issue with SBDH workflows we have been performing active user testing at ZSFG for over six months and have begun the process at UCSF this month. Our initial testing and interviews with subject matter experts suggests that social workers spend approximately 60 minutes per patient manually reviewing fragmented charts across multiple encounters to bolster their understanding of the patient’s social and behavioral needs and treatment history. With an average daily caseload of 10 to 15 patients per week, this represents 40 to 60 hours per week of highly skilled professional time spent on chart navigation rather than direct patient management. documentation, totaling 40-60 hours weekly. This significantly limits direct patient care. Additional time and effort is needed to then identify resources and makes referrals. Because of these workflows limitations we estimate that social workers are unable to participate in the care of 25% of patients on inpatients teams and many of these patients are at high risk of adverse outcomes because of social and behavioral needs. Thus this is a substantial problem. Through a human centered interative design process we believe we have developed a deployment strategy, outlined in our proposal, that complements their workflow, reduces cognitive burden and improves efficiency.
References
[1] Magnan, S. (2017). Social Determinants of Health 101 for Health Care: Five Plus Five. NAM Perspectives. Discussion Paper, National Academy of Medicine, Washington, DC. https://doi.org/10.31478/201710c
[2] https://qpp.cms.gov/docs/QPP_quality_measure_specifications/CQM-Measures...
[3] https://www.sf.gov/news-mayor-lurie-unveils-breaking-the-cycle-vision-fo...
[5] Gold, Rachel, et al. "Using electronic health record–based clinical decision support to provide social risk–informed care in community health centers: protocol for the design and assessment of a clinical decision support tool." JMIR Research Protocols 10.10 (2021): e31733.
[6] Yuan, Dong, et al. "Evaluate Summarization in Fine-Granularity: Auto Evaluation with LLM." arXiv preprint arXiv:2412.19906 (2024)
Comments
Love this concept Luke and
Love this concept Luke and team. Addressing social and behavioral needs is SO critical to patient health. I could see a tool like this creating efficiencies for our often over-extended clinical teams, including social workers and care coordination staff, as well as for our patients. In the interactive demo, I really like how there are embedded recommended actions to address social risks. Would love for our patients and teams to be able to benefit from this work.
This work has multiple
This work has multiple applications and can lead to interdisciplinary collaborations, even outside of inpatient hospital medicine. For example, it would be particularly useful in the emergency department, where time and human resources are scarce, and where we treat especially vulnerable populations with high rates of unmet social needs. This work would tie in nicely with my ongoing NIH-funded K23 research, which involves designing EHR-based clinical decision support tools to facilitate social risk-informed treatment for opioid use disorder.
Second this. We have rolled
Second this. We have rolled out the Social Work prioritization tool in the ED, but because there is less time for nursing to collect structured data in the ED, there are less triggers available to make the tool robust. This AI indicator would augment that work beautifully and provide a quick social and behavioral driver synopsis of the ED patient.
This study is an extension of
This study is an extension of research our team at SIREN has done in collaboration with OCHIN to develop clinical decision support tools that present social risk information to clinical teams in ways that make risk data usable and meaningful in care planning. The application of LLM will increase clinical team efficiency and, ideally, tool uptake. I do really think the pilot's iterative PDSA cycles are critical--they will help the team to design messages that clinical teams (SW + residents) believe have added value. That said, even co-designed CDS are not always used. In our original study, very few clinicians used the social SCDS tools. I really appreciate that the tools the team creates in this study might have different value for SW than for clinicians, which is why eventually I think qualitative research on tool impacts would be an interesting addition down the road. FWIW, I doubt the CMS screening positivity rates are going to budge, though I understand why you would measure them. Since I think the clinical outcomes are the important ones because as we have seen in the CMS Accountable Health Communities demonstration reports, changing social risk has not been the sole mediator for changing chronic disease outcomes. One other minor thing for team to consider: social workers might be asked to review a subset of charts to double check the rubric in primary outcome (ii). Excited to see what happens with this important work.
Thanks Laura! We are very
Thanks Laura! We are very excited for the potential of this being incorporated into Social Work APeX workflows. Social Work is already monitoring indicators, but we know the current non-AI tool is missing large portions of our population in need. Marrying the two is an exciting possibility. Our Social Workers would review the summary along with their chart review when a patient is flagged as high risk.
This initiative represents a
This initiative represents a substantial advancement in integrating AI into healthcare, enhancing the management of social determinants of health, and optimizing patient care. By utilizing the capabilities of large language models, the Whole Person Care Navigator will ensure that healthcare providers can focus more on direct patient care and less on administrative tasks, ultimately improving patient outcomes and overall healthcare efficiency.
As the medical director of
As the medical director of the Social Medicine team, this proposal would significantly improve the way our team functions, providing efficient, stream-lined, and patient-centered recommendations. The time and effort cut from searching through the EMR would be invaluable. It is one step to recognize social risk, but this proposal moves forward to CHANGING social risk. It is a remarkable addition to our current workflow in the emergency department, and I look foward to engaging with this tool to improve patient outcomes.
This is very exciting! This
This is very exciting! This project dovetails in elegantly with one of UCSF's key strategic priorities: addressing capacity and throughput. Senior leadership have already resourced a large project for Care Management Redesign that is using the medical record to screen admitted patients for Care Management needs (both Case Management and Social Work). The intent is to identify these patients as early in the admission as possible so that discharge planning can be more proactive. Identifying patients with social and behavioral drivers early is a critical piece of our new Social Work operating model. We have already launched a tool to search for structured social indicators, but for all the reasons you've stated, this information often only lives in unstructured data. Aligning these two efforts would greatly improve the chance of success of this executive project.
This Whole Person Care summary also addresses the gap we have in evaluating both Ambulatory and Emergency patients. There is often too little structured data on Emergency patients to fully trigger the Prioritization tool, and the tool does not apply to Ambulatory at all. This AI tool would go a long way to filling those gaps.
Thanks all for these
Thanks all for these constructive comments. We have made the following revisions to the proposal based on the feedback and comments:
We additionally appreciate the feedback about adding qualitative interviews to assess faciliators and barriers to use of the tool. Our build process includes interative human centered design with subject matter experts in the development phase and we have experience performing rapid qualitative interviews in the post deployment/optimaization phase. Therefore we could include this both for providers using the tool and for patients. Finally, given the flexibility and customization of this tool we agree that this could be expanded into the Emergency Department to assist with the management of opiate use disorder via the workflows currently being investigated by Dr. Molina.
Great proposal and Social
Great proposal and Social Work would support this. We have already discovered that single item screeners are not sufficient for us to get the most relevant psychosocial information about our patients. Being able to pull information from narrative documentation could potentially help us identify early which patient charts we should screen and prioritize for assessment.
This concept is fantastic.
This concept is fantastic. In the context of Social Work, I appreciate that it can not only speed up decting urgent issues, but may also be able to illumate trends or less spotlighted concerns that could benefit from supportive intervention (either psychosocial, or material resources). I woudl like to see if there is a way of identifying patients who are struggling to engage in care, summarize ED admission/visit trends, and summarize community programs/agencies/resources that the patient has engaged with prior. Looking forward to hearing more, and hope this proposal is among the selected for funding! I also appreciate the depth of thought and consideration given to assisting those in need.
Exciting idea. Have you done
Exciting idea. Have you done any user testing for the design? Will users find the additional information distracting and time-consuming to go through, or will it fit easily in their workflow and solve a problem they currently have?
Thank you for these questions
Thank you for these questions. Yes we have been performing active user testing at ZSFG for over six months and have begun the process at UCSF this month. Our initial testing and interviews with subject matter experts suggests that social workers spend approximately 60 minutes per patient manually reviewing fragmented charts across multiple encounters to bolster their understanding of the patient’s social and behavioral needs and treatment history. With an average daily caseload of 10 to 15 patients per week, this represents 40 to 60 hours per week of highly skilled professional time spent on chart navigation rather than direct patient management. documentation, totaling 40-60 hours weekly. This significantly limits direct patient care. Additional time and effort is needed to then identify resources and makes referrals. Because of these workflows limitations we estimate that social workers are unable to participate in the care of 25% of patients on inpatients teams and many of these patients are at high risk of adverse outcomes because of social and behavioral needs. Thus this is a substantial problem. Through a human centered interative design process we have developed a deployment strategy, outlined in our proposal, that complements their workflow, reduces cognitive burden and improves efficiency.
Incredibly innovative
Incredibly innovative proposal with clearly a great amount of thought behind it! SW resources are spread very thin with very limited capacity at our hospitals, yet they are being asked to respond effectively to increased social needs by our patients in part because of a higher number of SDOH screens being performed in our system. A way to centralize data and help prioritize and suggest interventions would be welcome for all providers aiming to tackle the diverse needs of our patient population. I do recommend being very thoughtful around issues of violence/abuse and incorporating IPV experts/SMEs (such as Dr. Leigh Kimberg and others) into the design process in order to prevent inadvertent sharing of sensitive data with inappropriate parties.
I am very supportive of this
I am very supportive of this proposal. As a clincal hospitalist and Medical Director for Value Improvement I have been involved in numerous cases in which delayed identification or resolution of unmet social needs have led to both prolonged hospital stay as well as challenges with efficient linkages to needed outpatient social resources. In our Parnassus Medicine UBLT we have identified challenges in expediting care delivery specific to the burden of identifying social needs given the current state of our medical record system has numerous episodes of care each with a wealth of relevant social information but are all unlinked, meaning it requires significant time for manual review to piece together a patient's story. A tool such as this could help address this issue for all care team members, not just social workers so that the medical team can be informed with the right information for careful planning of a patient's hospital and discharge needs. Moreover, the ability to show references to what the tool is finding is a big win to mitigate the risk of hallucinations and ensure that providers are comfortable that they know the source of information that is being summarized. Lastly, this tool has the opportunity to address one of the biggest challenges for hospitalist in addressing social determinants of health in the hospital: time. A survey we conducted in 2023 of 85 UCSF hospitalists found that lack of time was the biggest barriers to managing social determinants of health, and this tool has the ability to make the information gathering process significantly more efficent. I am strongly in support of this proposal.