1. What problem are you trying to solve?
In chronic autoimmune diseases, such as Myasthenia Gravis (MG), as in several other conditions across specialties, patients experience fluctuating symptoms and highly individualized disease courses. This leads to patients having numerous questions, and a high demand for information, with patients often getting overwhelmed and confused with numerous internet search results. Often patients relaize after their visit that they forgot to ask or clarify several questions pertaining to their diagnosis leading to new chains of messages .Access to sub specialized healthcare providers is significantly limited. While electronic health records (EHRs) such as Apex MyChart are an interface to bridge care gaps, frequent MyChart messages can overwhelm providers and staff.
One current approach by heath systems including UCSF health is to warn patients about possible charges when providers respond to myChart messages This may especially dissuade patienst from marginalzed socioecomic status from messaging providers .We thus propose a relational AI chatbot to reduce provider burnout and enhance patient care, by offering a reliable source of answers to patient questions about their specific diagnosis (s).
Effective education and support are crucial for patients with chronic autoimmune diseases to manage symptoms, adhere to treatment plans, and make informed lifestyle choices. Without targeted guidance, patients feel overwhelmed and disconnected from healthcare providers, leading to suboptimal outcomes. Lack of readily available guidance provokes anxiety with MyChart messages being one of the few available resorts. Additionally, reducing the burden on healthcare providers and their ancillary staff is essential for care quality and to prevent burnout.
Previous efforts have included telehealth-based education programs and mobile health (m-health) apps. However, these solutions often require high patient involvement and may not provide personalized, continuous support. Traditional educational methods like brochures and websites can lead to information overload, require fact-checking and do not offer answers tailored to individual questions.While APEX/EPIC allows providers to include disease-specific educational content in the After Visit Summary, the material is often too lengthy, making it difficult for patients to find key information—ultimately contributing to information overload. MyChart messaging thus remains the predominant method for patient provider communication outside of clinic visits, which tends to overburden health systems.
The primary end-users for this pilot project are patients with MG, particularly those newly diagnosed. Secondary end-users include healthcare providers, such as neurologists and specialists, who can leverage the relational AI chatbot to enhance patient education and engagement while managing their workload more effectively.
We will first pilot this for providers at UCSF health treating Myasthenia Gravis (MG). The tool and infrastructure can be extended and adapted to other automimmune diseases such as Multiple Sclerosis and Rheumatoid Arthritis.
2. How might AI help?
We propose the development and evaluation of a relational AI chatbot [1,2] aimed at delivering patient-centered education to support behavior change, improve disease literacy, and promote treatment adherence. This intervention is designed to enhance patient outcomes while alleviating the growing workload on providers and care teams tasked with responding to generic disease questions. In brief,this will make patient care more effecient and reduce redundancies.
AI chatbots have the potential to offer a promising scalable approach to supporting chronic disease management by offering flexibility and enabling reliable, equitable conversations. Research shows that patients often feel more comfortable disclosing sensitive information to nonjudgmental AI chatbots[3-5], leading to improved clinical outcomes. Unlike traditional one-way interventions, the chatbot gives patients more agency in their learning process. While delivering structured information, it adapts to patients’ needs, answering questions, directing them to verified sources, and connecting them with healthcare providers as needed.
We will develop the chatbot through a phased, safety-first approach using GPT-4 via Azure OpenAI, which offers secure, HIPAA-aligned infrastructure. In Phase 1, we will curate a trusted knowledge base drawing from UCSF-approved materials, validated educational sources, and original content authored by Dr. Paul. In parallel, we will compile approximately 100 high-quality doctor–patient conversations to support few-shot prompting and our retrieval-augmented generation (RAG) system. This foundation will enable the chatbot to generate accurate, contextually grounded responses in a patient-friendly tone aligned with institutional standards.
In Phase 2, we will implement key guardrails, including confidence thresholds that trigger fallback responses or human referrals when uncertainty is detected, as well as a human-in-the-loop review process to audit interactions and inform iterative improvements. In Phase 3, we plan to explore deployment on fine-tunable architectures (e.g., open-source LLMs) to further enhance domain adaptation while preserving transparency, interpretability, and clinical safety. This modular development strategy allows us to launch with a robust, secure system and expand its capabilities responsibly over time.
Ultimately, this innovation can pave the way for disease-specific modules and educational materials across multiple chronic autoimmune diseases that patients (through their providers) can avail upon diagnosis, engage in conversations over the initial 3-6 months to enhance their disease knowledge, and management skills. This can potentially reduce some messaging volume on myChart which currently represents a huge burden for UCSF health as well as other tertiary health systems. After successful deployment in Myasthenia Gravis clinics at UCSF Health, our medium-term vision extends to applying this relational AI chatbot to other chronic autoimmune conditions especially ALS and Rheumatoid Arthritis where disease knowledge and management efficacy and skills are critical. This approach ensures that patients are not only informed but also feel supported and motivated throughout their healthcare journey, ultimately driving better outcomes.
3. How would an end-user find and use it?
The AI chatbot would be integrated directly into APeX MyChart, the same interface that patients use to send messages to their providers. Once a patient receives a confirmed diagnosis, the provider would inform them about the AI chatbot and its capabilities. If the patient agrees, the chatbot can be enabled for them from the “Wrap-Up” section, allowing them to begin using it immediately. Patients would interact with the chatbot through text-based conversations within APeX MyChart, receiving real-time responses and support. They could also connect with healthcare providers if needed, ensuring that the chatbot complements rather than replaces direct provider communication. The AI support would be most useful during the initial diagnosis and early stages of disease management, when patients are seeking information about the disease and guidance for daily life. By being embedded in APeX MyChart, the chatbot becomes a seamless part of the patient's existing communication and management tools.
Our proposed chatbot will have three core capacities: education, relational engagement, and persuasive (nudging) abilities. These are grounded in Co-PI Zhang's AI Chatbot Behavior Change Model[1] and the RESPECT model [2] from UCSF for improving patient-provider communication. The chatbot will provide comprehensive information on MG symptoms, medications, side effects, and early warning signs, while fostering a supportive relationship to boost patient confidence and behavioral efficacy. It will also offer practical guidance for symptom monitoring and daily challenges at home and work and suggestions in the realm of preventive health.Further it will provide links to direct patients to reliable physician trusted sources such as Myasthenia Gravis foundation of America (MGFA).
4. Embed a picture of what the AI tool might look like.
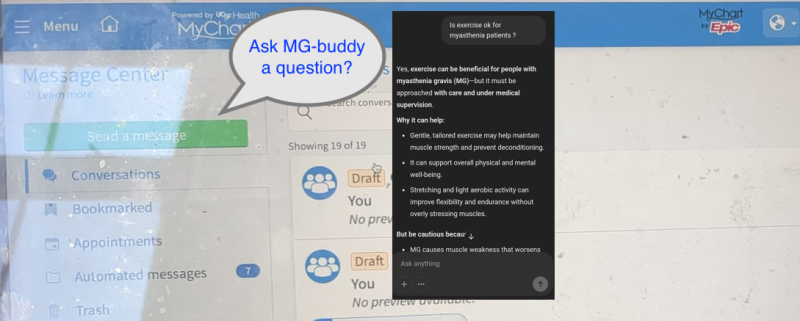
Figure 1: A simple illustration of a patient logging in to MyChart and being prompted to chat with the AI chatbot within the message center. And an example of a message exchange where a chatbot answers their question.
5. What are the risks of AI errors?
Potential AI errors include false positive or false negative predictions, and "hallucinations" from generative AI models. False positives could lead to unnecessary anxiety or interventions, while false negatives might result in missed symptoms or delayed treatment. Hallucinations could provide incorrect or misleading information. To measure and mitigate these risks, we would implement continuous monitoring and validation of the AI outputs, involve healthcare professionals (specialty physicians) in reviewing critical information, and provide clear disclaimers about the AI's limitations. Regular feedback from users would also help identify and address errors. The first 10 patients using the chatbot will be the PI’s own clinic patients and then in 3 months will offer other MG providers. While it engages users in interactive, personalized conversations, the chatbot will be programmed to deliberately defer any questions related to acute symptom management, emergencies, or health crises—promptly advising patients to call 911 or contact their healthcare provider. It will also include routine reminders encouraging patients to message their care team if their questions are not fully addressed, reinforcing that the chatbot is intended as an educational tool rather than a substitute for clinical care.
6. How will we measure success?
We will take a multipart approach to measure the success of the AI chatbot incorporating both patient and provider feedback as well as log data analysis from Apex. In the initial phase, we will conduct feasibility testing to assess technical stability, response accuracy, and integration within clinical or research workflows.
a)Physician and Patient Feedback: In one-on-one interviews, physicians will respond to questions about their enthusiasm for using the tool, their ability to provide it to patients, and their perception of whether the tool has the potential to reduce the provider and staff burden of responding to messages.Since the pilot is aimed at Myasthenia Gravis patients, in a short patient survey, specific measures will be used to assess patients' confidence in disease knowledge, symptom awareness, and treatment adherence, along with a scale to measure patients' satisfaction with the chatbot,their willingness to continue using it and whether the chatbot helps answer questions they would otherwise want to reach the provider for. These surveys can be integrated into mychart.
b)Outcome Metrics based on log data analysis from Apex:
(i)Reduction in Provider Messages: Analyzing “provider-patient dyads", we will measure the reduction in MyChart messages received by providers’ offices, comparing data before and after AI chatbot implementation doing both "within provider" and "between providers" analyses.
(ii)Predictors of Bot Usage: We will assess factors predicting greater usage of the bot to ensure typical health disparities based on race, ethnicity and gender are not exacerbated.
(iii)Healthcare Utilization: We will compare measures such as ER visits, hospital admissions, and urgent care visits over a one-year period to assess tangible reductions.
(iv)Evidence for Leadership: We will analyze data showing increased patient engagement, improved health outcomes, reduced provider messages, and positive feedback from users to convince UCSF Health leadership to continue supporting the AI implemenntation.
Abandonment Criteria: If the AI fails to improve patient outcomes, shows high rates of errors, or receives consistently negative feedback, we will consider abandoning the implementation
7. Describe your qualifications and commitment:
PI Dr. Pritikanta Paul is a Neuromuscular Neurologist and currently a Health Sciences Assistant Professor of Neurology at the UCSF. His specific clinical and research interests lie in immune mediated muscle and nerve diseases. His recent experiences of seeing medically underserved patient populations, have led to an interest in health disparities as they affect outcomes in neuromuscular diseases and he recently developed an educational intervention utilizing text messages in improving outcomes of myasthenia gravis.
Co PI: Dr. Jingwen Zhang, Associate Professor,Dept of Communication,also affiliated withDepartment of Public Health Sciences at University of California Davis (UCD). Dr. Zhang’s research focuses on understanding, designing, and testing emerging persuasive technologies in shaping public health attitudes and behaviors. Her research has been supported by NIH, USDA, Robert Wood Johnson Foundation, and University of California. During the past five years, she has focused on understanding and developing conversational AI or chatbot in persuasion and health promotion. She has collaborated with scholars from UCSF’s School of Nursing to develop an AI chatbot for promoting physical activity, and is currently working on developing a chatbot to promote heart health awareness and knowledge among underserved minority women in the U.S.
This project directly aligns with research priorities for both the PI and Co-PI. Both PIs are committed to dedicating effort to this project, participating in regular work-in-progress sessions, and collaborating with the Health AI and AER teams for development and implementation of the AI algorithm.The PI Dr. Paul has the assurance of release time from their academic department.
References
1. Zhang J, Oh YJ, Lange P, Yu Z, Fukuoka Y. Artificial Intelligence Chatbot Behavior Change Model for Designing Artificial Intelligence Chatbots to Promote Physical Activity and a Healthy Diet: Viewpoint. J Med Internet Res. 2020 Sep 30;22(9):e22845. doi: 10.2196/22845. PMID: 32996892; PMCID: PMC7557439.
2. Mutha, S., Allen, C. & Welch, M. (2002). Toward culturally competent care: A toolbox for teaching communication strategies . San Francisco, CA: Center for Health Professions, University of Californ ia, San Francisco.
3. Lee, Y. C., Yamashita, N., & Huang, Y. (2020). Designing a chatbot as a mediator for promoting deep self-disclosure to a real mental health professional. Proceedings of the ACM on Human-Computer Interaction, 4(CSCW1), 1-27.
4. Branley-Bell, D., Brown, R., Coventry, L., & Sillence, E. (2023). Chatbots for embarrassing and stigmatizing conditions: could chatbots encourage users to seek medical advice?. Frontiers in Communication, 8, 1275127.
5. Liang, K. H., Shi, W., Oh, Y. J., Wang, H. C., Zhang, J., & Yu, Z. (2024). Dialoging resonance in human-chatbot conversation: how users perceive and reciprocate recommendation chatbot’s self-disclosure strategy. Proceedings of the ACM on Human-Computer Interaction, 8(CSCW1), 1-28. doi: 10.1145/3653691
Comments
I'm very interested in your
I'm very interested in your ideas, but it will take a lot of development and testing before there is a chatbot that UCSF would feel comfortable setting loose to talk with patients without a human in the loop. Will you use Versa? Have you started doing any prompt engineering to give the LLM some context and instructions? Will you plan to use retrieval augmented generation (RAG) to restrict responses to a specific set of approved informational materials about Myasthenia Gravis? Or some other method?
Thanks Mark. Very valid
Thanks Mark. Very valid questions. I think the plan is to have human oversight for a long time, just hoping that we need it less and less over time, but continue to have the option for patients to reach out to providers directly.
We have revised the answers to the second question (how will AI help?) with more elaboratation on the various development and testing phases.