GPT-4-DCS: A Large Language Model Pilot to Reduce Hospital Discharge Summary Documentation Burden and to Enhance Quality and Safety
Section 1. The UCSF Health Problem
Section 1. The UCSF Health Problem
Sedation planning is an essential step in the endoscopy preprocedural workflow. Triage of which patients require higher levels of anesthesia support is critical to maximize patient safety and allocate limited anesthesia resources. Current workflow for sedation triage decisions requires significant manual chart review by administrative staff and clinicians. This project aims to develop “GIVersa-Endoscopy,” a custom LLM-powered assistant to augment the sedation triage process for endoscopic procedures at UCSF Health. Integrated into existing clinical workflows, this AI assistant will streamline decision-making and reduce administrative burdens. While this assistant is initially focused on gastroenterology-specific procedures, the administrative challenges and importance of peri-operative sedation triage are widespread across the health system in many divisions, highlighting the larger potential uses for an AI-based sedation triage assistant.
Section 1. The UCSF Health problem.
The UCSF Office of Population Health (OPH) Complex Care Management (CCM) team provides advanced care management services to adult patients with high medical and/or psychosocial complexity who are high utilizers of inpatient or emergency department (ED) services. The CCM program involves essential high-touch support such as assessing individual patients’ healthcare challenges, developing targeted care plans, providing health education and coaching, coordinating linkage to care, and connecting to other community resources. Prior analysis of this program’s outcomes showed a statistically significant decrease in ED and observation encounters for patients enrolled in the program. The impact of this program therefore has significant potential to help address UCSF Health’s current ED crowding and bed capacity challenges, reduce readmission rates, and help meet quality metrics associated with specific patient populations.
Currently, one of the most time-consuming challenges faced by the CCM team is determining individual patient eligibility for the CCM program. Despite using a reporting workbench that identifies patients meeting initial objective criteria, the team must still manually chart review to determine eligibility, which can consume up to 30 minutes per patient. This manual process can also be inconsistent, as it has been noted that different reviewers assess medical and social complexities differently based on their training and clinical background.
The UCSF Health Problem
We aim to automate specialty-specific chart review, a high provider burden, error-prone process that costs clinicians 15–45 minutes per patient, leading to 6–12 hours of weekly administrative overhead contributing to pajama time. This burden impairs clinic throughput, contributes to burnout, and compromises care quality, especially in specialties like Gastroenterology where fragmented, longitudinal data including scanned outside records are the norm.
1-The UCSF Health Problem
At UCSF and other leading academic medical centers, the referral intake and triage process for new patients is strained, leading to long delays and high rates of incomplete referrals.
The UCSF Health problem
Inflammatory bowel disease (IBD), including Crohn's disease and ulcerative colitis, is a chronic inflammatory condition affecting 1.5 million people in the United States, with a significant hospitalization rate of 9.24 per 100 IBD patients annually [1]. Flares of the disease are a common cause of these hospitalizations. Optimal management of acute IBD flares necessitates timely surgical consultations, endoscopic evaluations, initiation of anticoagulant therapy, and possible surgical interventions [2]. However, adherence to these protocols is often compromised by heavy clinical workloads and oversight, leading to delays that diminish patient care quality, extend hospital stays, and increase healthcare costs [3].
UCSF, a tertiary medical center with a comprehensive IBD program, is committed to providing extensive care for patients with complex IBD cases necessitating hospitalization due to flares. Strict adherence to clinical protocols is vital for enhancing the quality of patient care, reducing the duration of hospital stays, and decreasing healthcare costs [3]. Despite these high standards, adherence to these protocols at UCSF, particularly at newly integrated sites such as Saint Francis Memorial Hospital and St. Mary's Medical Center, and during the absence of clinical fellows who assist the service, can fall short of expectations. This is largely due to the challenges posed by heavy clinical workloads and oversight.
How might AI help?
Our goal is to enhance the Advancing Patient-Centered Excellence (ApeX) electronic medical records (EHR) system at UCSF to improve monitoring and management of patients admitted with IBD flares. By integrating large language model (LLM) AI tools, such as VERSA at UCSF, both structured data (e.g., orders, lab values) and unstructured data (e.g., physician notes) collected during patient admissions can be effectively processed. This AI tool will actively monitor adherence to the established IBD management protocol and alert gastroenterology/IBD providers and primary team providers, such as hospitalists, by displaying a reminder window when they access a patient’s chart in the ApeX EHR system and being available as SmartPhrases available to providers when writing notes and signing off to the next provider in the hand-off in the APeX EHR system. This prompt aims to prevent delays in care by ensuring timely adherence to necessary clinical actions.
Key Areas Where AI Is Essential:
How would an end-user find and use it?
Our objective is to enhance the Advancing Patient-Centered Excellence (ApeX) electronic medical records (EHR) system at UCSF, aiming to improve the monitoring and management of patients admitted with IBD flares. By incorporating large language model (LLM) AI tools, such as VERSA at UCSF, we can effectively process both structured data (e.g., orders, lab values) and unstructured data (e.g., physician notes) collected during patient admissions. This AI tool will actively monitor adherence to the established IBD management protocol. It will alert gastroenterology/IBD providers and primary team providers, such as hospitalists, by displaying a reminder window when they access a patient’s chart in the ApeX EHR system. Additionally, SmartPhrases will be made available to providers for use when writing notes and during the hand-off process to the next provider, ensuring seamless communication. These prompts are designed to prevent delays in care by ensuring timely adherence to necessary clinical actions.
Embed pictures of what the AI tool might look like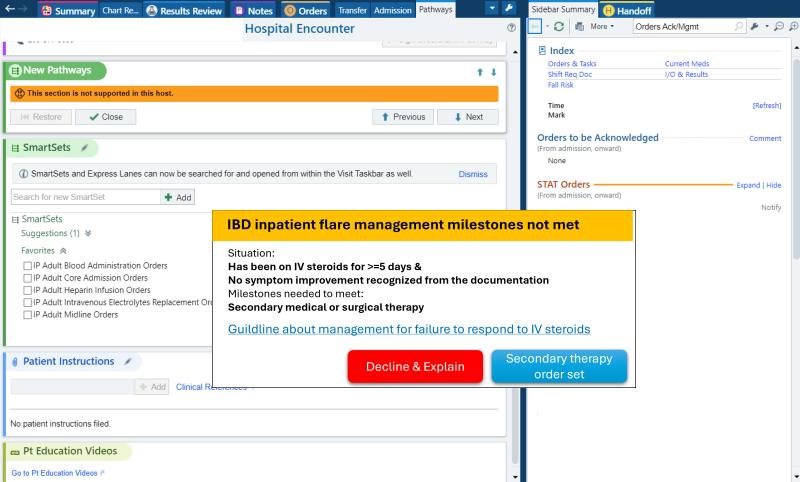
Figure 1 shows the reminder window for the IBD flare inpatient milestone not met: Failure to response to the first line therapy, but no secondary medical or surgery therapy started. The failure and is recognized by the AI tools, large language model, from the unstructured data, symptoms included in the provider and nurse notes. The deficiency of secondary medical or surgery therapy information is collected from structured data, medication orders, and notes, notes documenting surgical evaluation and procedure plan. A useful link is also attached to show the most updated guideline about the milestones for user education. And if the provider accepts it, it will open an order set directly for the convenience. But it does not force the provider to take any action, in case it is a falsely positive reminder. It works more as a reminder and allow the provider to check. The “Decline” button will allow the user to leave a comment to help with the tool.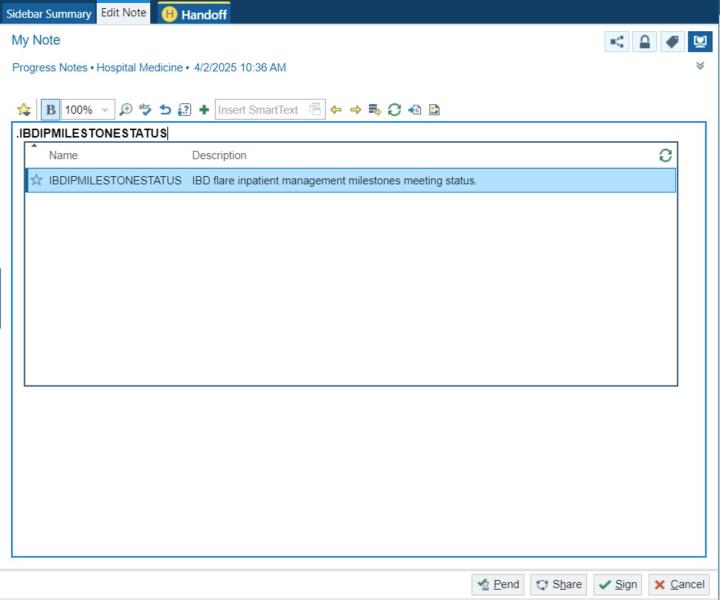
Figure 2 depicts a SmartPhrase that shows the current IBD flare inpatient milestone meeting status. It will contain following menus to allow the provider to select if necessary and allow the provider to do any edits. The SmartPhrase will also work in the Handoff part for the purpose of signing off and providing information for other teams, like the night on call shift or other consult teams.
What are the risks of AI errors?
AI tools may occasionally misinterpret data or generate errors, leading to false positives or false negatives. For instance, a milestone may not be met, yet the AI might incorrectly indicate that it has been met (false positive). However, this is unlikely to cause additional harm, since a provider who would have recognized the unmet milestone independently would not be misled into overlooking it simply because the AI suggested otherwise. The only scenario in which a milestone would still be missed is if both the provider and the AI tool fail to recognize it—essentially the same outcome as not using the AI tool at all. Conversely, the AI might fail to recognize that a milestone has been met, resulting in a false negative. However, these errors can often be corrected through provider review. Given that these milestones are generally straightforward for providers to verify, but may be overlooked due to heavy clinical workloads, the AI tool primarily functions as a reminder rather than a decision-maker.
How will we measure success?
The implementation and evaluation of the AI tool for IBD flare management necessitate a strategic approach to measure its effectiveness and minimize disruption of clinical workflow and maximize provider adoption and satisfaction. The evaluation process will be structured into two primary components:
Existing APeX Data Metrics: Protocol Adherence, Hospital Stay Duration.
Additional Ideal Metrics: Health Costs, User Feedback, and Scoring.
Describe our qualifications and commitment
This project is spearheaded by Yuntao Zou, MD, a seasoned hospitalist with extensive experience in inpatient medical management. Dr. Zou is also an accomplished AI researcher, with a clinical and research focus on leveraging AI tools, such as Large Language Models (LLMs), to enhance healthcare delivery and clinical decision-making processes. I am responsible for designing and overseeing the entire project process. If selected, I will devote at least 10% or as required effort for 1 year to ensure the success of this proposal.
Vivek Rudrapatna, MD, PhD, serves as the co-lead for this initiative, with a specific focus on enhancing the IBD management protocol and developing the AI tool. As a physician-scientist and specialist in inflammatory bowel disease, Dr. Rudrapatna brings a wealth of experience in IBD management. He also leads a research group dedicated to developing methods for analyzing healthcare data, aiming to enhance clinical decision-making processes.
The UCSF Health problem: Hospital discharges are among the most vulnerable transitions in patient care, where errors and miscommunication can lead to missed follow-up, patient harm, and readmissions. National data has shown that nearly 1-in-5 Medicare patients are readmitted within 30 days of hospital discharge, often due to missed appointments, unfilled prescriptions, or unrecognized clinical deterioration (Jencks et al., NEJM 2009;360:1418-28).
Section 1. The UCSF Health Problem
Diagnostic error, the failure to establish or communicate an accurate and timely explanation of a patient’s health problem, affects 12 million people in the U.S. annually, leading to delays in treatment, potentially avoidable healthcare utilization, and increased morbidity and mortality.1